Improving Safety - SEA
Significant Event Audit
Improving the quality and safety of patient care is the duty of all healthcare professions (see ABC of Patient Safety No 1). They all should acquire the competency of practice review in light of endorsing good practices and remedying poor performance.
Significant event audit (SEA) is a form of qualitative audit where healthcare professionals discuss together as a team events in a structured manner that they consider important to patient care and safety with the ultimate aim of improving the quality and safety of the care they offer.
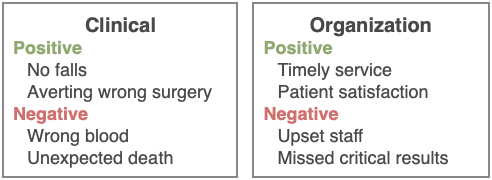
SEA draws on the Pendleton approach, in which both positive and negative aspects of practice are considered for audit. Positive achievements are acknowledged and rewarded which in turn facilitates a constructive approach when negative situations are audited.
SEA can be implemented through the following steps:
Consideration of events for audit
Any event thought by any team member to be significant for the care and safety of patients or the conduct of practice should be open for consideration. However, teams are advised to give some consideration to the events they would want to analyse before starting to use SEA. A good idea is to begin with a core list of events that has been developed by the team and to refine it according to evolving local needs and interests. It is important to realize the importance of creating a balance between positive and negative events and frequent and infrequent events in order to maintain an interest in the SEA process within the workplace.
Examples of significant events
Identification of events for analysis
Having agreed upon a list, mechanisms are needed within the practice to ensure the listed events are spotted and prioritized. This can be done through creating a paper or computer-based registry with regular reminders. Dedicated staff can be informed about events and consulted on suitability of certain events for SEA.
Information gathering
Adequate data should be collected on the event so the team can determine what happened, how it happened and why it happened. Sources of data include 5Ps: People, Paper, Place, Process, Paradigm (working climate). However, much of the information will be found in people’s heads. The use of pre-designed forms will ensure consistency in data collection. The individual(s) involved, directly or indirectly, in the event may be best placed to lead the investigation, but others can also be delegated this task.
Team-based meeting
The central component of SEA is the team meeting held to discuss events. Beyond discussing what happened, how it happened and why it happened, a key function of the meeting is to consider the implications of the event on the quality and safety of care and make appropriate policy changes that lead to significant improvements.
The meetings should be held at a known time and place, have a clear agenda, have a designated leader, be of reasonable length, lead to clear decisions, and should be documented to ensure sustainability.
The meetings should be conducted in an open and non-threatening atmosphere. Failure to do so will hamper the entire SEA process. Where there is fear or blame, team members will become reluctant to engage and will most probably withhold important information or even events. The greatest resource in terms of knowledge, understanding, skills, innovation and effectiveness is the team itself.
Analysis of event
What happened?
Data gathered by the investigating team from various sources should give enough information on the nature of the event and how it happened. The investigating team should present the data in an orderly fashion, supported by tables or graphs where appropriate.
Why it happened?
Team members should then try to answer the question “why it happened?” by identifying the underlying factors, whether positive or negative, that led to the event. Utilising a standard analysis framework over the meetings is recommended. Common frameworks usually include factors such as patient factors, staff factors, team factors, task factors, environmental factors, and administrative factors.
What was learnt?
The team, through group reflection, should reach conclusions as to whether the event was due to local factors or other wider systemic factors. The team should reflect on their performance as a whole and whether enough support or recognition was offered to those involved in the event. It is also important for the team to realize the state of desired competencies among team members that are essential for safe quality care.
What will change?
Change is not always required, especially when reflecting on positive events. On the other hand, negative events may necessitate changes in the way things are done to ensure they do not recur. Such changes may include modifications in the process of care, introduction of new risk assessment tools, development of a patient engagement program, teamwork training, conducting quantitative clinical audit, or improvement in the use of informatics.
Implement and monitor
Any agreed upon actions should be implemented by staff assigned to co-ordinate and monitor change in the same way a unit or department would act on the results of quantitative audits. Progress with the implementation of necessary change should always be monitored by placing it on the agenda of future SEA meetings.
Share and review
Sharing SEA reports, including implemented changes, with colleagues and leadership should be part of the wider framework of clinical governance. This can only happen within a culture that is open and fair where staff feel comfortable to speak and discuss their performance as long as they are not violating norms or taking unnecessary risks. Creating this culture and protecting it is the duty of all staff at all levels.
Reporting events
Healthcare systems should encourage confidential and anonymous reporting of incidents that cause no harm, or where harm was averted (near miss), or that cause harm for learning and performance improvement purposes. Events that cause serious harm should also have a separate accountability path that does not cross with the learning path.
Reading Material
-
- Pendleton D,et al. The Consultation: An Approach to Learning and Teaching. 1984. Oxford, Medical Publications.
- Pringle M, et al. Significant event auditing. Occas Pap R Coll Gen Pract. 1995;70:1-71.
- NPSA. Significant Event Audit. 2008.