IPPSEP Framework
Patient Safety
Most high-risk industries have succeeded in controlling their hazards and have significantly improved their safety levels over the years. However, healthcare systems are still struggling with an unacceptable percentage (10%-20%) of patients being harmed while receiving care. Furthermore, at least half of these adverse events are considered by safety experts to be preventable (50%-90%).
System Redesign
International and national healthcare bodies are calling for system redesign as a strategy to improve patient safety. Such calls include adoption of principles of good governance, prioritizing safety as a system aim, integrating safety and quality initiatives in the care of patients, availably and utility of performance information, developing individual and organizational learning skills, working in teams, and empowering patients and their families along their healthcare journey.
Preparing Healthcare Professionals
In order to create the right organizational culture and working climate, that are both essential for the desired system change, we need healthcare professionals who have acquired through their education and training a core of knowledge, skills, and attitudes (competencies) that will enable them to deliver safe, effective and patient centered care.
In its new vision for healthcare professionals education, The National Academy of Medicine (formerly Institute of Medicine) states that all healthcare professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics.
Furthermore, the World Health Organization has emphasized the importance of inter-professional education and collaborative practice as a strategy for overcoming health system fragmentation and preparing health professionals to work inter-professionally as effective members of healthcare teams.
InterProfessional Patient Safety Education and Practice
In adopting such recommendations, we present an InterProfessional Patient Safety Education and Practice (IPPSEP) framework that endorses the concept of learning and working together for patient safety. The framework can be utilized when developing patient safety curricula that are suitable for all professions and when guiding health professionals to collaborate to deliver safe care.
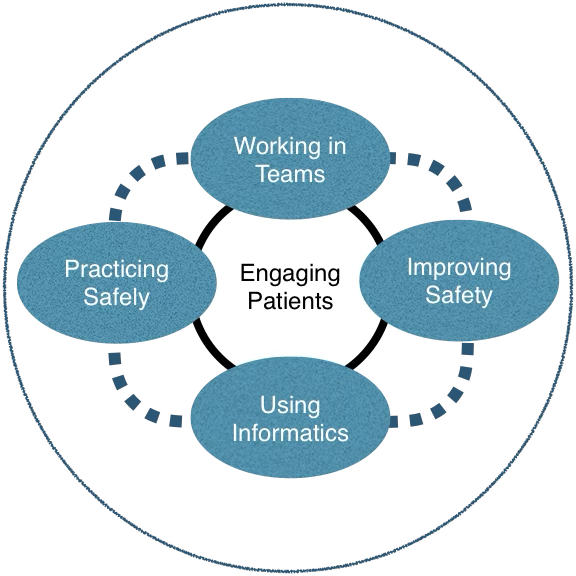
At the center of this framework is an empowered patient capable of sharing knowledge and decisions with health professionals. The framework emphasizes that safe care is delivered through teams that learn and work inter-professionally and through the utilization of information and related technology in their decisions. The framework supports the acquisition of competencies related to delivering safe care and to continuously improve care safety by all health professions.
Patient Engagement
Engaging patients through knowledge, consultation, and involvement can help create an environment where health professionals and patients can partner to make healthcare safer. Informed patients better understand healthcare-related risks and can help minimize their occurrence during their care journey. Patients have first hand experience of the healthcare system and are in a position to give valid advice to make services safer. Health professionals should know how to engage patients and how to establish partnerships based on respect and compassion.
Working in Teams
Integrated care requires health professionals to work in teams. True teams need members who know their roles and responsibilities, respect those of others, and support each other to deliver safe effective care. Teams also need to know how to collaborate with other teams along the patient journey. Cooperation, communication, conflict resolution coordination, coaching, and cognition are all acquired teamwork skills that all healthcare professionals should acquire.
Informatics
The use of computer hardware and software in processing of data, information and knowledge, especially for communication and decision-making, has been associated with a reduction in medication error and adverse events and improvement in compliance with clinical practice guidelines. The use of information technology to minimize risk exposure and improve patient outcome and safety is conditioned by its safe design and proper use.
Practicing Safely
Health professionals, regardless of their discipline, need to acquire principles of safe practice along the patient care pathway. This should include agreed-upon practices related to diagnosis, risk assessment, medication and invasive procedures. This consensus will create a shared understanding between healthcare professionals on how to safely care for their patients.
Improving Safety
Healthcare professionals are accountable for their performance and for continuously improving the quality and safety of the services they offer. This requires healthcare professionals to acquire a set of abilities regarding the appreciation of systems, understanding practice variation, learning through incremental practice improvement, and understanding the human side of change.
This framework is an adoption of the Academy of Medicine core competencies that all clinicians should possess, regardless of their discipline, to the field of patient safety. We believe that this framework can contribute to interprofessional education and collaborative practice in the field of patient safety. The framework is not meant to be an exhaustive list of competencies nor a list of competencies to the dedicated patient safety specialist. The framework is directed to all clinicians to help them work in teams offering safe care to their patients. The framework can also be utilized by regulatory and oversight authorities to ensure appropriate health professions education and safe healthcare delivery.
Reading Material
-
- Towards eliminating avoidable harm in health care. Global patient safety action plan 2021-2030. WHO. 2021.
- Health Professions Education: A bridge to quality. Institute of Medicine. 2003.
- Framework for action on Interprofessional education and collaborative practice. WHO. 2010.
- Campanella P, et al. The impact of electronic health records on healthcare quality: a systematic review and met analysis. Eur J Public Health. 2016:26:60-4.